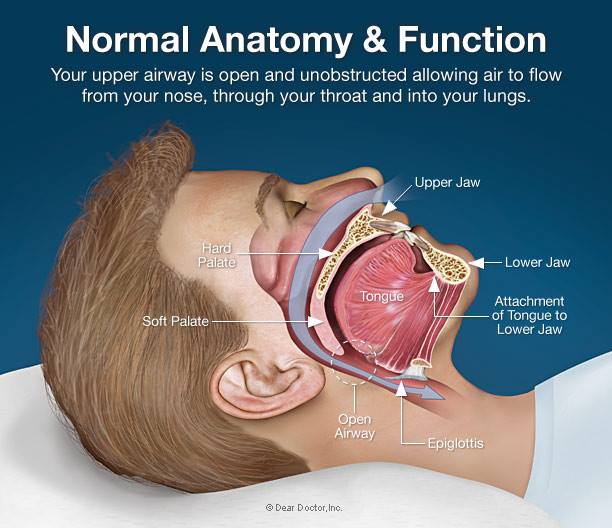
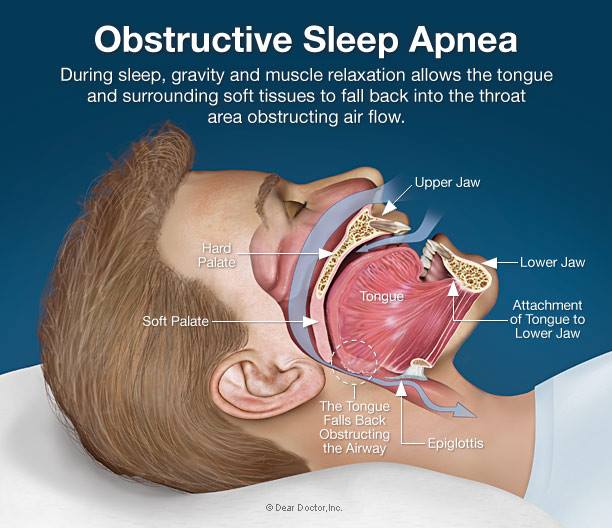
Approximately one in every seven adults experience sleep-disordered breathing (SDB) Sleep-disordered breathing is characterized by numerous, brief (10 second or so) interruptions of breathing during sleep. These interruptions, which usually occur when relaxation of the upper airway muscles decreases airflow, lower the level of oxygen in the blood and, as a result, affected individuals are frequently aroused from deep sleep as they struggle to breathe.
Symptoms of sleep-disordered breathing include loud snoring and daytime sleepiness. The most common form is SDB is Obstructive Sleep Apnea (OSA).
OSA can occur in men, women and children of all ages and sizes. Most people who have OSA do not realize they suffer from the condition. Often, it is someone else who witnesses the first signs of OSA.
The signs and symptoms of obstructive and central sleep apneas overlap, sometimes making the type of sleep apnea more difficult to determine. The most common signs and symptoms of obstructive and central sleep apneas include:
Consult a medical professional if you experience, or if your partner observes the following:
Many people don't think of snoring as a sign of something potentially serious, and not everyone who has sleep apnea snores. But be sure to talk to your doctor if you experience loud snoring, especially snoring that's punctuated by periods of silence.
Ask your doctor about any sleep problem that leaves you chronically fatigued, sleepy and irritable. Excessive daytime drowsiness (hypersomnia) may be due to other disorders, such as narcolepsy.
People who sleep next to a snorer have more pain, higher levels of fatigue and sleepiness and may even be at higher risk for hearing loss, according to two recent studies. Complaints of snoring and apnea have risen sharply in recent years along with the general increase in obesity, a risk factor for sleep problems. Research shows:
People who sleep next to snorers may wake up as often during the night as people with documented sleep disorders.
One Mayo Clinic study found that spouses of snorers woke at least partially an average of 21 times an hour, nearly as often as the 27 times the snorers were awakened by their documented sleep problem.
Spouses of snorers and people with sleep apnea complain of excessive daytime sleepiness and fatigue, which can affect relationships at both work and home.
Sleep apnea may occur if you're young or old, male or female. Even children can have sleep apnea. But certain factors put you at increased risk:
Risk Factors
Excess weight. Fat deposits around your upper airway may obstruct your breathing. However, not everyone who has sleep apnea is overweight. Thin people develop the disorder, too. Snoring (Snoring can cause the soft palate to lengthen, which in turn can obstruct the airway)
Neck circumference. The size of your neck may indicate whether or not you have an increased risk of sleep apnea. That's because a thick neck may narrow the airway and may be an indication of excess weight. A neck circumference greater than 17.5 inches (44 centimeters) is associated with an increased risk of obstructive sleep apnea.
High blood pressure (hypertension). Sleep apnea is not uncommon in people with hypertension.
A narrowed airway. You may inherit a naturally narrow throat. Or, your tonsils or adenoids may become enlarged, which can block your airway.
Being male. Men are twice as likely to have sleep apnea as women are. However, women increase their risk if they're overweight, and the risk also appears to rise after menopause.
Family history. If you have family members with sleep apnea, you may be at increased risk.
Other disorders and syndromes. Hypothyroidism, acromegaly, amyloidosis, vocal cord paralysis, post-polio syndrome, neuromuscular disorders, Marfan's syndrome, and Down Syndrome.
Other physical conditions. Conditions such as immune system abnormalities, severe heartburn or acid reflux and high blood pressure. It isn't clear whether the conditions are the cause or the result of sleep apnea.
Use of alcohol, sedatives or tranquilizers. These substances relax the muscles in your throat.
Smoking. Smokers are three times as likely to have obstructive sleep apnea as are people who've never smoked. Smoking may increase the amount of inflammation and fluid retention in the upper airway. This risk likely drops after you quit smoking.
Heart disorders. People with atrial fibrillation or congestive heart failure are more at risk of central sleep apnea.
Stroke or brain tumor. These conditions can impair the brain's ability to regulate breathing.
What happens if I do not treat my sleep apnea? Sleep apnea is considered a serious medical condition. Left untreated, complications may include:
Cardiovascular problems. Sudden drops in blood oxygen levels that occur during sleep apnea increase blood pressure and strain the cardiovascular system. If you have obstructive sleep apnea, your risk of high blood pressure (hypertension) can be up to two to three times greater than if you don't. The more severe your sleep apnea, the greater the risk of high blood pressure.
Stroke. Obstructive sleep apnea also increases the risk of stroke, regardless of whether you have high blood pressure. People with sleep apnea are three times more likely to suffer a stroke or die, compared to people in a similar state of health but without sleep apnea.
Daytime fatigue. The repeated awakenings associated with sleep apnea make normal, restorative sleep impossible. People with sleep apnea often experience severe daytime drowsiness, fatigue and irritability. You may have difficulty concentrating and find yourself falling asleep at work, while watching TV or even when driving. You may also feel irritable, moody or depressed. Children and adolescents with sleep apnea may do poorly in school or have behavior problems.
Traffic accidents. Studies have shown that patients with OSA perform poorly on driving simulation tests and have an accident rate 2-7 times as high as people without OSA.
Sleep-deprived partners. Loud snoring can keep those around you from getting good rest and eventually disrupt your relationships. It's not uncommon for a partner to go to another room, or even on another floor of the house, to be able to sleep. Many bed partners of people who snore are sleep deprived as well.
Memory problems, depression and other complications. People with sleep apnea may also complain of memory problems, morning headaches, mood swings or feelings of depression, a need to urinate frequently at night (nocturia), and impotence. Gastro esophageal reflux disease (GERD) may be more prevalent in people with sleep apnea. Children with untreated sleep apnea may be hyperactive and may be diagnosed with attention-deficit/hyperactivity disorder (ADHD).
Complications with medications and surgery. Obstructive sleep apnea is also a concern with certain medications and general anesthesia. People with sleep apnea may be more likely to experience complications following major surgery because they're prone to breathing problems, especially when sedated and lying on their backs. Before you have surgery, tell your doctor that you have sleep apnea. Undiagnosed sleep apnea is especially risky in this situation.
Type II Diabetes. Recent reports have indicated that the majority of patients with type 2 diabetes also have obstructive sleep apnea (OSA). Data suggests that OSA is also independently associated with alterations in glucose metabolism and places patients at an increased risk of the development of type 2 diabetes.
How is OSA treated? For milder cases of sleep apnea, your doctor may recommend lifestyle changes such as losing weight or quitting smoking. If these measures don't improve your signs and symptoms or if your apnea is moderate to severe, a number of other treatments are available. Certain devices can help open up a blocked airway. In other cases, surgery may be necessary.
Treatments for obstructive sleep apnea may include:
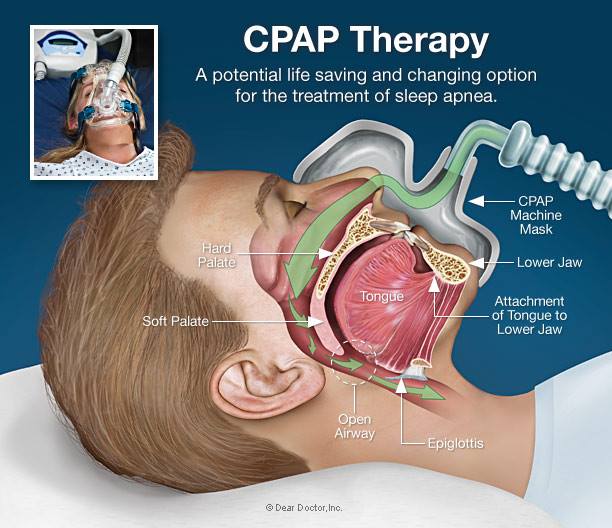
Continuous positive airway pressure (CPAP). If you have moderate to severe sleep apnea, you may benefit from a machine that delivers air pressure through a mask placed over your nose while you sleep. With CPAP (SEE-pap), the air pressure is somewhat greater than that of the surrounding air, and is just enough to keep your upper airway passages open, preventing apnea and snoring.
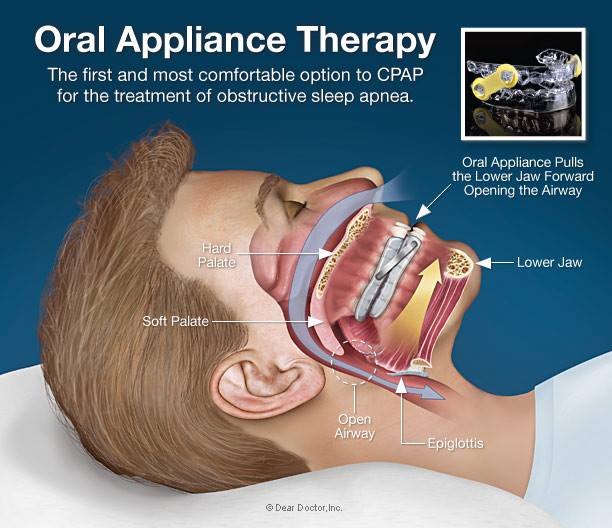
Although CPAP is a preferred method of treating sleep apnea, some people find it cumbersome or uncomfortable. In fact, many sleep apnea patients are experiencing even greater success with the use of an oral appliance such as the OASYS.
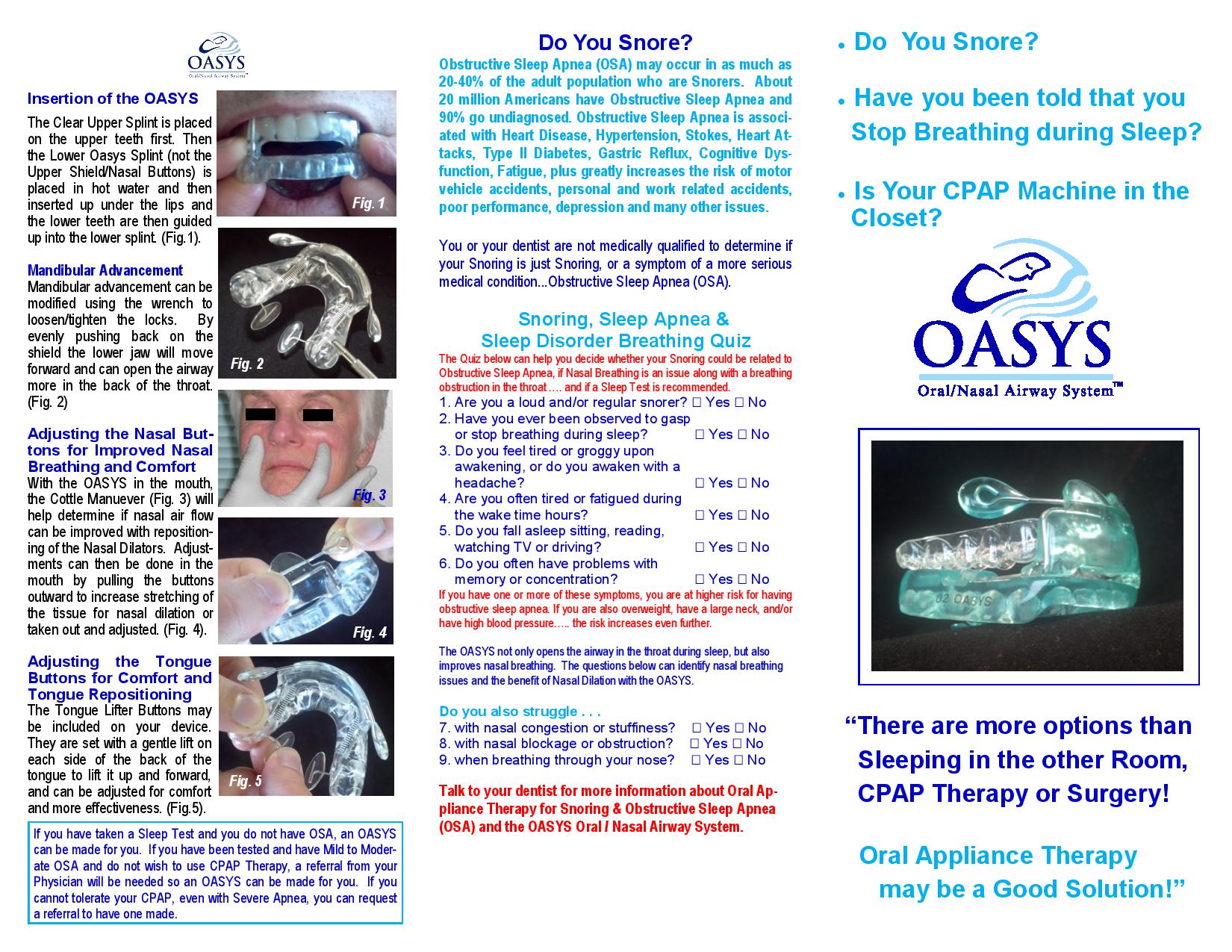
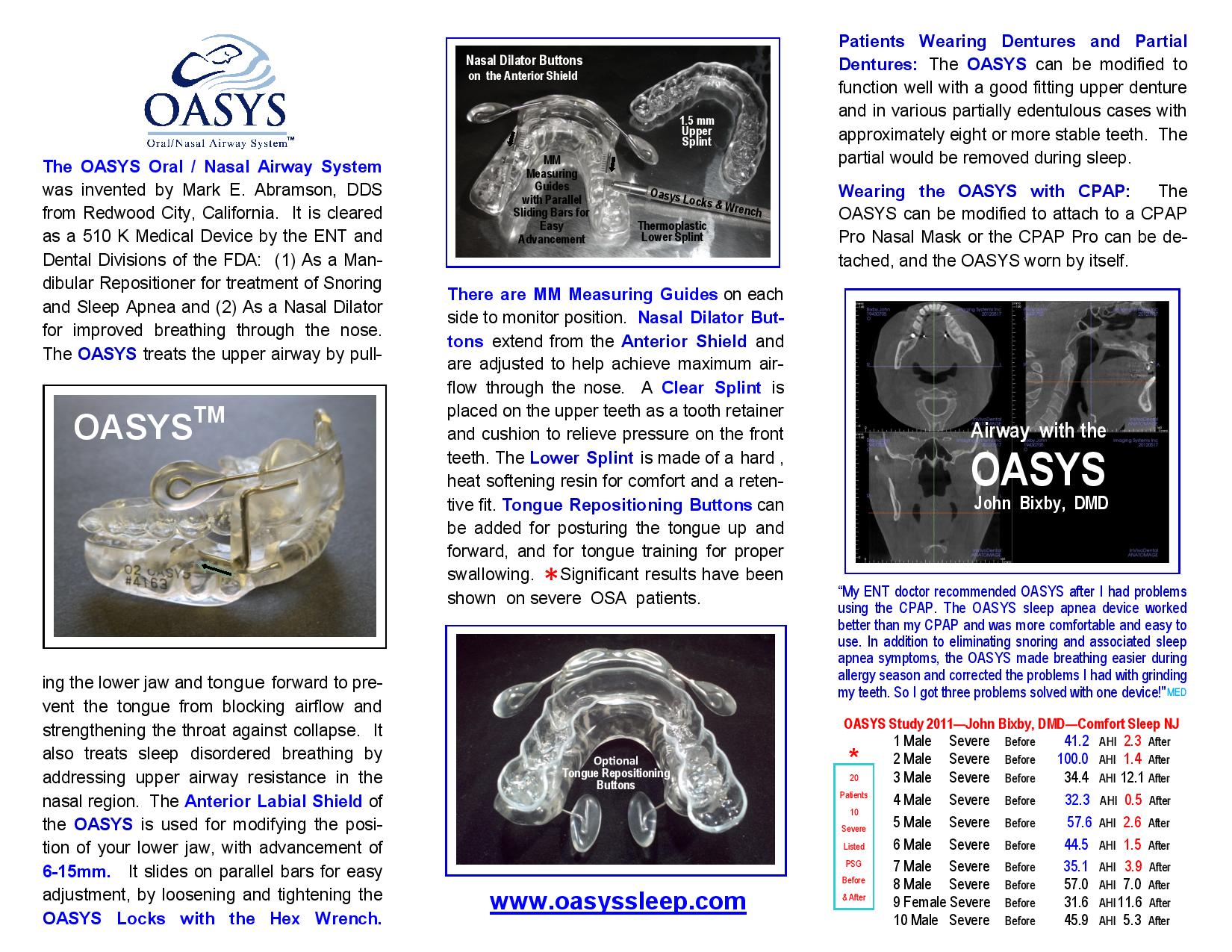
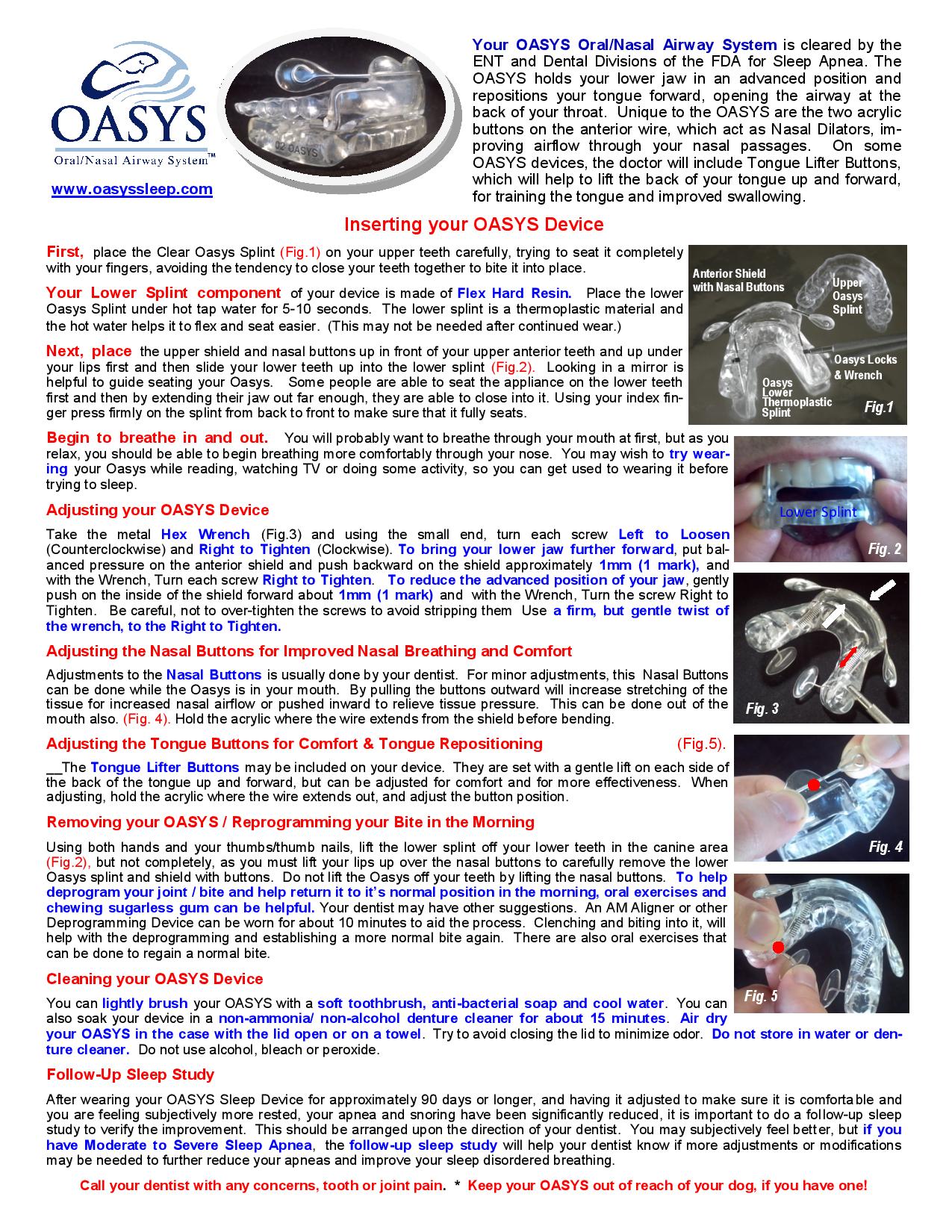
Oral appliances. Another option is wearing an oral appliance designed to keep your throat open. CPAP is more effective than oral appliances, but oral appliances may be easier for you to use. The OASYS is the first dental device to address both vulnerable regions of the respiratory tract. By repositioning the mandible it holds the lower jaw forward to keep open the pharyngeal area in back of the tongue. Acting as a nasal dilator, it decreases airway resistance so it improves ease of airflow through the nasal passage.
Benefits of dental devices such as the OASYS seem to offer the following benefits:
Dental devices have also shown better long-term control of sleep apnea when compared to uvulopalatopharyngoplasty (UPPP), the standard surgical treatment. There are also few complications with a dental device.
Surgery
The goal of surgery for sleep apnea is to remove excess tissue from your nose or throat that may be vibrating and causing you to snore, or that may be blocking your upper air passages and causing sleep apnea. Surgical options may include the following: uvulopalatopharyngoplasty, maxillomandibular advancement, nasal surgery and tracheostomy.

For years CPAP has been the standard treatment for obstructive sleep. Previously, most respiratory physicians would prescribe nightly use of the CPAP for the treatment of OSA. This method involves wearing a facemask connected to a pump that forces air into the air passages while the patient sleeps. The pressure of the machine is set high enough to overcome any obstruction.
However, it has drawbacks, including discomfort from the mask, a dry or stuffy nose, and eye irritation. CPAP treatment for OSA is only effective if the patient is willing to use the device. Unfortunately, due to the often uncomfortable and invasive nature of this treatment method CPAP has a relatively low compliance rate ranging from 40% to 70%.
Many patients find this treatment uncomfortable or intolerable and seek an alternate treatment method such as the OASYS.
The OASYS Oral/Nasal Airway System™ is the only dental device to treat both vulnerable areas of the upper airway, the nasal and oropharyngeal, with one patented system. The OASYS Oral/Nasal Airway System™ strengthens the throat area by pulling the lower jaw and tongue forward to prevent the tongue from blocking the airflow and strengthening the throat against collapse.
The OASYS Oral/Nasal Airway System™ is the only dental device for treatment of snoring and obstructive sleep apnea that has the capacity to open the path of air through the nose. The patented device uses buttons under the lips which create a gentle stretch of the upper lip region and puts traction on the inner nasal tissue to dilate the nose. This increases the nasal volume and reduces the resistance of airflow an average of 50.
Ask yourself these questions:
Do you suffer from sleep apnea or snore but have found using the CPAP to be cumbersome and uncomfortable?
Do you travel frequently and find it difficult and cumbersome to bring your CPAP with you?
Do you find it difficult to become intimate with people because you sleep with a mask and tubing on your face and a machine by your bedside?
Does the CPAP interfere with your bed partner having a peaceful and restful sleep?
Is your CPAP machine collecting dust because you have stopped using it?
If you have answered yes to any of these questions, then the OASYS Oral/Nasal Airway System may be just the product you need to sleep with ease all night long.
Continuous Positive Airway Pressure
Before the advent of Oral Appliance Therapy, Continuous Positive Airway Pressure (CPAP) was the primary non-surgical method for treating Obstructive Sleep Apnea. CPAP works by delivering continuous air pressure into the airway, thereby keeping it open while the patient sleeps. The pressure prevents the airway from collapsing either fully or partially.
CPAP machines include the machine itself, a mask that fits over the nose and/or mouth, and a tube that connects the mask to the machine. CPAP still remains the primary treatment for patients with Severe Obstructive Sleep Apnea, while Oral Appliance Therapy is used as a first line of treatment for mild-to-moderate cases. However, if a patient with Sever OSA tries to use CPAP but cannot tolerate it, then Oral Appliance Therapy can be used as an alternative treatment modality at that point.
CPAP is an effective treatment for patients who can tolerate it. However, many patients still find CPAP difficult to tolerate due to feelings of claustrophobia and inability to sleep because of the noise from the machine and discomfort from the mask. There have been advances in CPAP technology over the years to make it more comfortable, including built-in humidifiers, auto pressure regulators and different kinds of machines and masks. It is important for patients and their doctors to take the time to find the device and settings that work best. Some patients simply cannot tolerate CPAP, effectively ruling it out as a treatment option.
Tips for Sleep Apnea Patients
Obstructive sleep apnea can be very serious. However, following an effective treatment plan can often improve your quality of life quite a bit. Treatment can improve your sleep and relieve daytime tiredness. It also may make you less likely to develop high blood pressure, heart disease, and other health problems linked to sleep apnea. Treatment may improve your overall health and happiness as well as your quality of sleep (and possibly your family's quality of sleep). 1 If you have been diagnosed with sleep apnea, the National Institutes of Health, the National Heart, Lung and Blood Institute and Mayo Clinic recommends you do the following:
Ongoing Health Care Needs
How Can Family Members Help?
Often, people with sleep apnea don't know they have it. They're not aware that their breathing stops and starts many times while they're sleeping. Family members or bed partners usually are the first to notice signs of sleep apnea.
Family members can do many things to help a loved one who has sleep apnea: